ARTICLE AT A GLANCE
Are Continuous Glucose Monitors (CGMs) the tech device of the future?
In short, yes, and perhaps it is only a matter of time before glucose tracking becomes as widely available as activity trackers.
Why? Poor blood sugar control impairs the gut and increases the risk of disease and cancer.
A CGM is a beneficial tool to collect data to personalize a diet, lifestyle and quality of life.
How is blood sugar affected by someone’s individual response to foods?
On a macro-level, someone’s carbohydrate tolerance, meaning how comfortably someone can eat a lower or higher carbohydrate diet, is unique to the individual.
Age, activity levels, metabolic health, genetics and insulin resistance play into the amount of carbohydrates someone tolerates. However, research can agree, a moderately lower carb diet made up of real food compared to the Standard American Diet (SAD) is favorable on blood sugar levels/control.
On a micro-level, blood sugar levels can spike beyond optimal ranges based off gut integrity and immunogenetic response to food. For example, as someone with an auto-immune disease and therefore some form of leaky gut, when I consume a healthy food like spinach, regardless of the low carb content, this vegetable irritates my gut and creates havoc on my blood sugar as shown on my CGM.
Identifying how certain ingredients spike my blood sugar allows me, and can allow anyone using a CGM, to personalize their diet to meet their needs of their physiology.
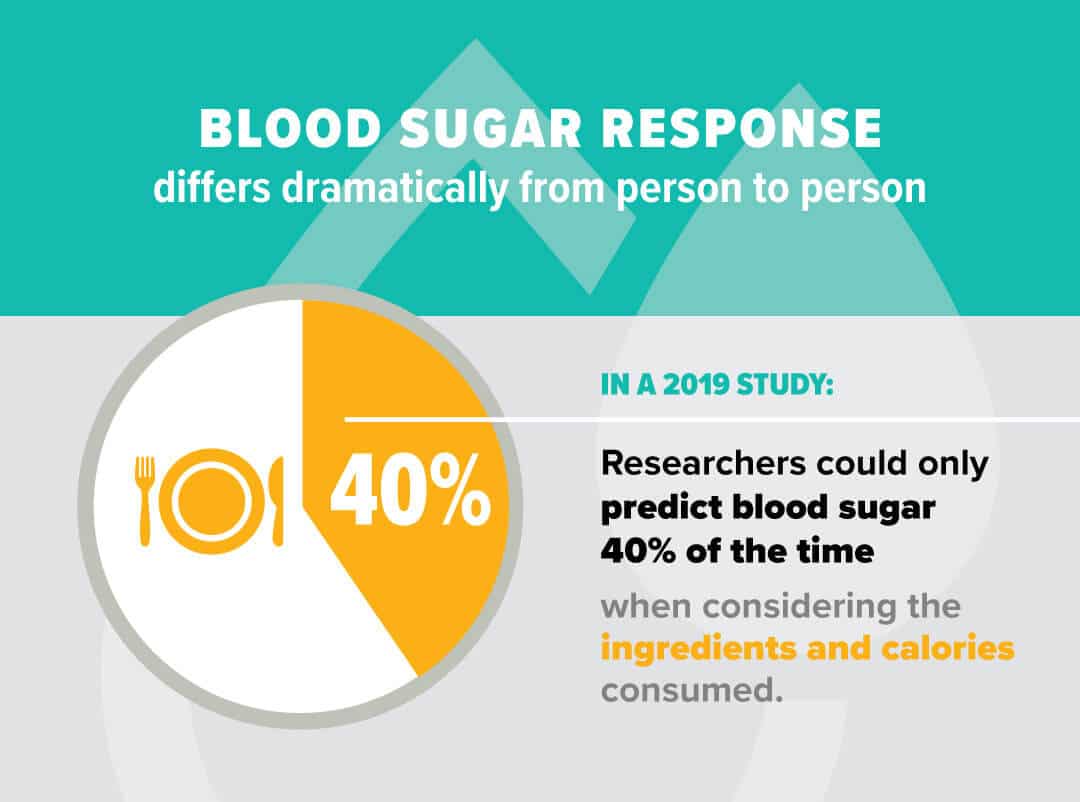
A 2019 study on non-diabetics, published in JAMA proved that when it comes to blood sugar control, we need to look at this full picture. Over 6 days researchers tracked glycemic responses to food in 300 participants and found that they could only predict blood sugar, at best, 40% of the time when considering the consumed ingredients and calories consumed by the participants. Yet, when the researchers factored in the specific composition of the microbiome of the individual, they were able to accurately predict blood glucose response 62% of the time.
CGMs help highlight that food is not just calories. Food is information that can help us get by or thrive. When we identify the right ingredients for ourselves, for our gut, for our blood sugar, it is then we feel our best, fight disease and inflammation, and heal our body from the daily stressors we are exposed to and improve our longevity and quality of life.
How important is tracking blood sugar to improve health?
Glucose tracking can help people understand their health, from diet to exercise and energy levels, to identifying habits that facilitate or inhibit health goals.
Blood sugar control either supports or hurts the gut microbiome. The stance of the gut predicts disease and longevity and the better our blood sugar control, the better outcomes we have with health.
Low blood sugar isn’t any better than high blood sugar as they both have their drawbacks. Low blood sugar can cause brain fog, confusion and even unconsciousness. High blood sugar causes oxidative stress, which can damage cells and nerve endings. Research has even shown that uncontrolled blood sugar, even in individuals without diabetes can lead to poor health outcomes including dementia.
What are the advantages of a CGM over fasting blood sugar testing and labs?
Wearing a CGM can facilitate the effort for someone who wants to hack their diet, blood sugar control and overall health.
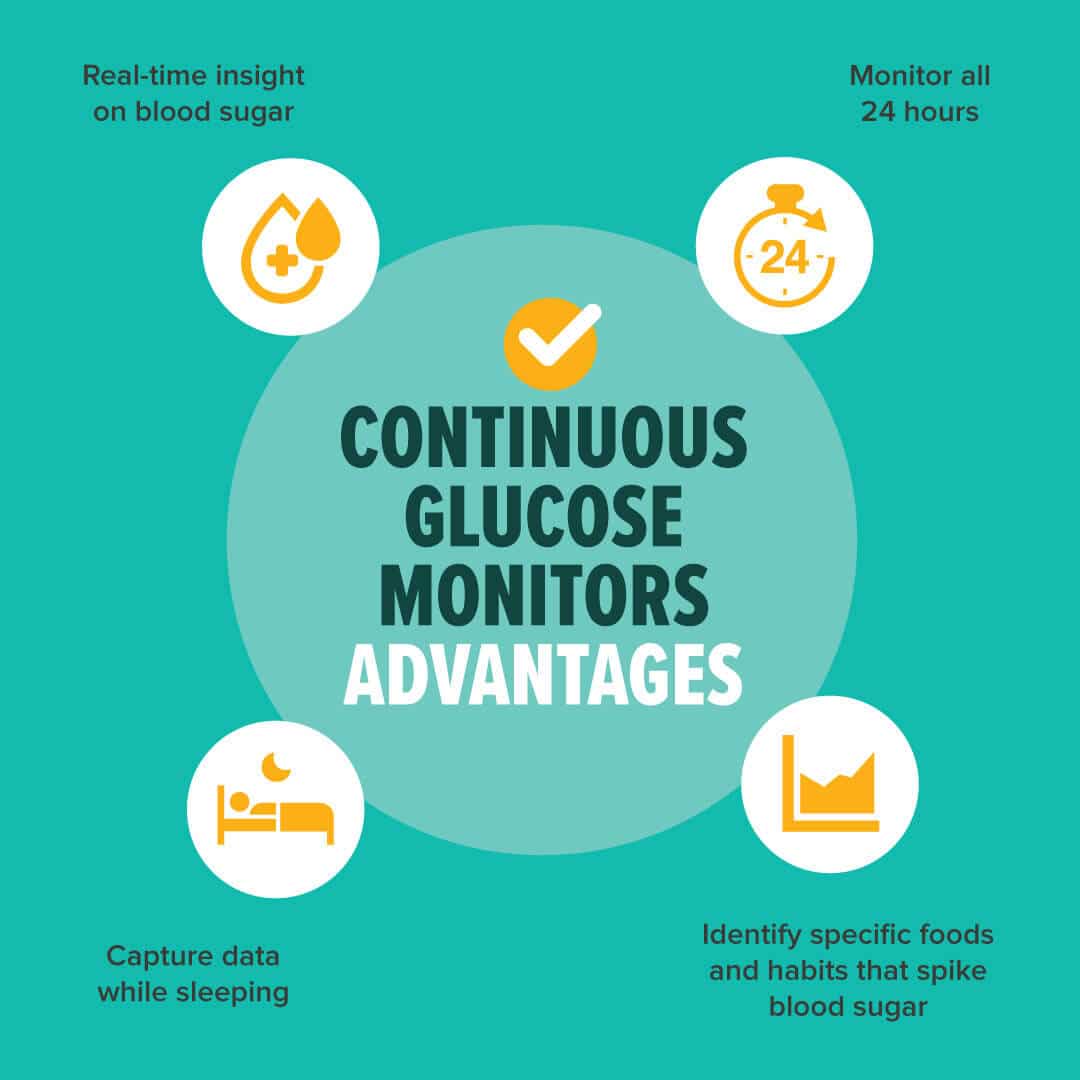
This technology can go beyond a single blood sugar reading that a blood glucose meter provides. A CGM can provide “real time” insight on whether a blood sugar is trending up or down.
Best of all, a CGM can capture data while sleeping, which is a common time when blood sugars fluctuate with other metabolic processes and circadian rhythms.
A CGM can be a key player in preventative medicine pinpointing lifestyle factors and foods that spike blood sugars and foods that likely have an immune response in an individual.
Many annual labs can include an A1C%, which is a value of an average of an estimated 3-month blood sugar reading. While A1C% labs are insightful and used in diagnosing someone with pre-diabetes or diabetes, it’s an average. An A1C% won’t identify if someone has swinging blood sugar readings or if they are steady. It does not capture a blood’s “time in range,” which is becoming the more common measurement of predicting someone’s blood sugar control.
Both an A1C and glucose meter are helpful tools but they do not measure glycemic fluctuations like a CGM is able to do.
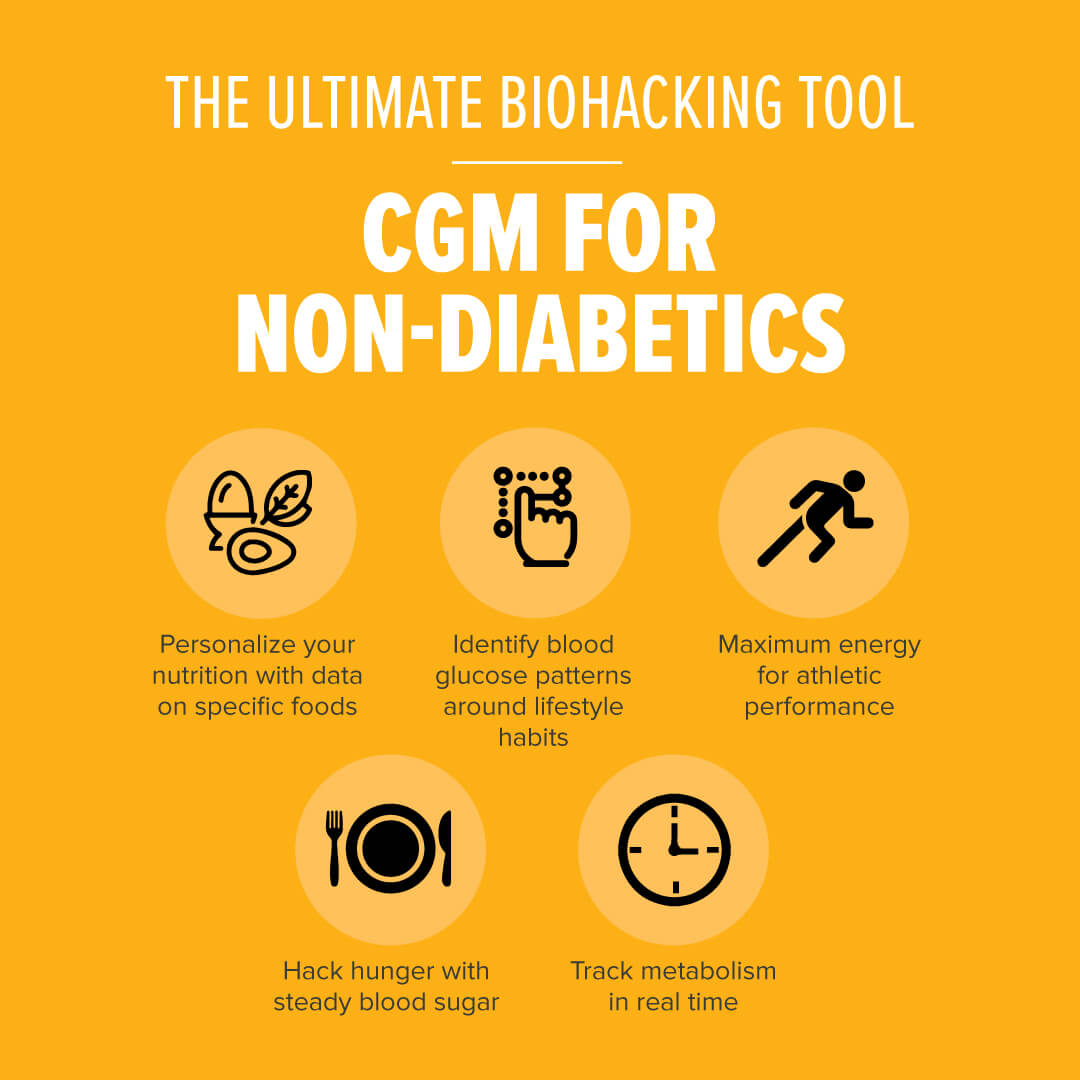
What are the benefits of using a CGM for non-diabetics?

- Personalized nutrition, meaning someone can identify how they body handles a certain food shortly after eating it and for the following hours.
- Identifies blood glucose patterns that relate to mealtime and lifestyle.
- CGM information can help people who are at risk of diabetes or heart disease.
- Improvements in blood sugar can be a key player for athletes looking to maximize their energy for a workout and performance.
- https://blog.mymetabolicmeals.com/wp-admin/edit.php?post_type=postDieters can hack hunger by maintaining steadier blood sugar levels throughout the day.
- CGMs offer a way of tracking your metabolism in real-time.
What does a non-diabetic CGM wearing biohacker have to say after wearing a CGM?
A client, we will call him Russell, shares his feedback on his process of getting a CGM and his top takeaways:
- The CGM required a prescription. My doctor had no problem writing a one-year script once I was clear that it was for experimentation and that I was happy to pay out of pocket.
- I used my phone and the app as the monitor, so only bought sensors. They came in a two-pack for about $150.
The 3 biggest takeaways from the experiment were:
- It doesn’t take much sugar for a glucose spike—a couple cookies and BOOM! This could be tempered by some activity in the 30-90 minutes after consumption (e.g., a good afternoon walk).
- Other carbs weren’t too bad for my levels as long as I didn’t eat too many or combine them with a big meal (as noted next).
- Combining carbs with a big meal—especially a high fat meal—always led to my biggest spikes. For example, if I had a “slow-carb” burrito bowl (beans, meat, veggies, guacamole, no rice) and also had some chips, my glucose would have a big spike. Some chips on their own were nothing major for me.
Kelly Schmidt, RD, LDN is a Type 1 Dietitian speaker and coach, providing practical solutions and personalized nutrition.






