Going gluten-free to support gut health isn’t just a trend — there’s real science behind it. You’ve probably seen “gluten-free” or “GF” labels on food products and wondered: What exactly is gluten? Gluten is a protein found in wheat, barley, and rye. It’s what gives baked goods their structure, elasticity, and chew. You’ll commonly find it in foods like bread, pasta, pastries, breaded meats, beer, and even in some sauces and dressings.
In this blog, we’ll explore how gluten can affect gut health, why removing it might be the key to resolving both gut and non-gut related symptoms, and how to successfully make the transition to a gluten-free lifestyle.
Gluten and Intestinal Permeability
One important way that gluten can impact gut health is through its role in intestinal permeability, commonly known as “leaky gut syndrome.” Specifically, a component of gluten called gliadin triggers the release of a protein called zonulin, which regulates the tight junctions in the intestinal lining. Elevated zonulin levels increase intestinal permeability, meaning the gut barrier becomes more “leaky.”
When this happens, substances like food proteins, toxins, and bacteria can pass from the gut into the bloodstream, which can activate the immune system and drive inflammatory processes. Increased intestinal permeability has been linked to a higher risk of autoimmune diseases, metabolic conditions like type 2 diabetes, neuroinflammatory disorders such as depression and Alzheimer’s, allergies, skin issues, and mast cell activation syndrome (MCAS).
This mechanism also explains why many people who undergo food sensitivity testing show sensitivities to multiple foods. It’s often not a true allergy or sensitivity; instead, proteins from these foods can leak into the bloodstream due to a compromised gut barrier.
Research shows that this process is most prominent in celiac disease, but it can also occur in individuals without celiac disease, such as those with non-celiac gluten sensitivity (NCGS).

Celiac Disease vs. Non-celiac Gluten Sensitivity
Celiac disease is an autoimmune disorder triggered by consuming gluten. Over time, the immune response causes inflammation that damages the lining of the small intestine. This damage leads to poor absorption of vital vitamins and minerals, as well as digestive symptoms like diarrhea and bloating.
Non-celiac gluten sensitivity (NCGS), on the other hand, occurs in individuals who don’t have the autoimmune condition but still experience symptoms after eating gluten. These symptoms can include bloating, abdominal pain, diarrhea, and constipation, as well as non-digestive issues like fatigue, headaches, brain fog, and joint pain. Reactions in NCGS can happen anywhere from hours to days after gluten ingestion, making it challenging to pinpoint gluten as the cause.
Unlike lactose intolerance, which results from a lack of the enzyme needed to digest lactose sugar, gluten sensitivity involves an immune response to the gluten protein, specifically gliadin. Because of this immune involvement, even very small amounts of gluten can trigger symptoms. In fact, several double-blind, placebo-controlled studies have shown that low doses of gluten (as little as 2 to 5 grams, roughly half a slice of bread) can provoke both gastrointestinal and systemic symptoms in people with NCGS.
Molecular Mimicry
Beyond its role in increasing intestinal permeability, gliadin has also been shown to contribute to a process called molecular mimicry. This occurs when a foreign substance shares structural similarities with the body’s own tissues, causing the immune system to mistakenly attack healthy cells. Research has identified a connection between gliadin and thyroid tissue, suggesting that gluten consumption may trigger or worsen autoimmune attacks on the thyroid by increasing antibodies such as TPO and thyroglobulin.
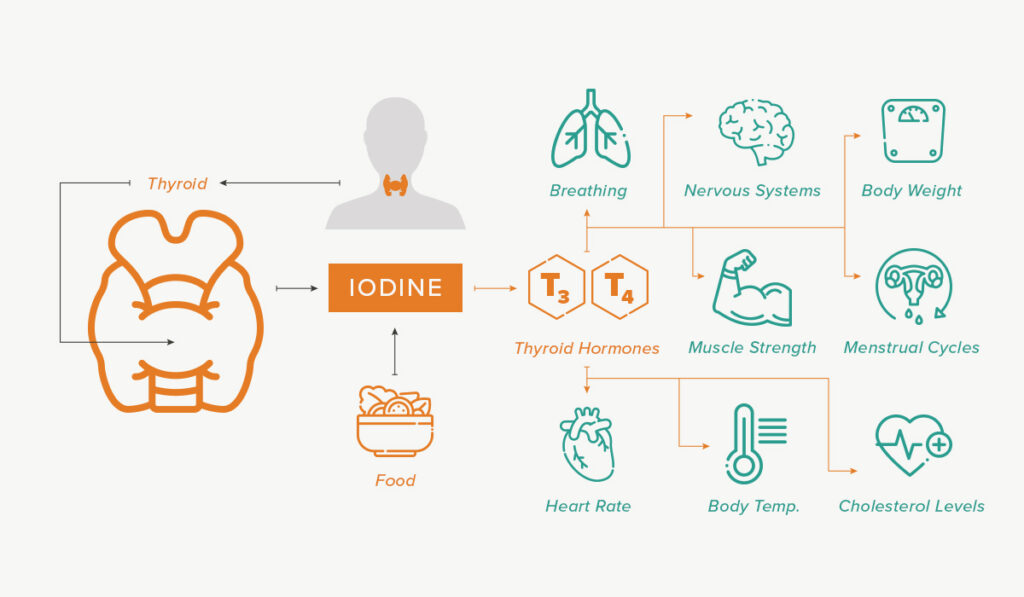
The Gluten-Thyroid Autoimmunity Connection
Moreover, studies have found that individuals with thyroid autoimmune conditions like Hashimoto’s often experience reductions in thyroid antibodies and a decreased need for thyroid medication (levothyroxine) after six months of following a gluten-free diet. Several factors could explain these improvements, including healing of the intestinal lining, the reduction of molecular mimicry-driven immune responses, and positive changes in the gut microbiome—possibly linked to lower glyphosate exposure.
Gluten & Glyphosate
Glyphosate exposure is another important reason why going gluten-free can benefit gut health. Glyphosate is the active ingredient in the herbicide Roundup. It is widely used on crops like wheat, corn, and soy in the United States. On wheat, it’s often applied as a pre-harvest desiccant to dry the crop and make harvesting easier. According to USDA residue testing, glyphosate residues have been detected in approximately 30–90% of wheat- and oat-based products, varying by region and brand.
Glyphosate acts like an antibiotic by killing beneficial gut bacteria such as Lactobacillus, Bifidobacterium, and Enterococcus. These are microbes that are essential for maintaining a healthy gut microbiome. These bacteria support immune function, regulate metabolism, and help control inflammation. Research shows that glyphosate disrupts gut flora balance and can reduce the production of short-chain fatty acids (SCFAs), which are crucial for metabolic health. SCFAs regulate appetite hormones, improve insulin sensitivity, and help reduce fat storage.
Going Gluten-Free
While celiac disease affects about 1% of the population, non-celiac gluten sensitivity (NCGS) is estimated to impact up to 10%. If you’re experiencing gut-related symptoms like bloating, diarrhea, or abdominal discomfort—or non-digestive symptoms such as brain fog, joint pain, elevated thyroid antibodies or systemic inflammation—it may be worth trying a gluten elimination trial to see if gluten could be a trigger.
Because reactions to gluten can be delayed and even tiny amounts may provoke a response, it’s best to fully eliminate gluten during this time. To truly evaluate how your body reacts, commit to removing gluten 100% from your diet for at least 3–4 weeks. This allows time for inflammation to subside and symptoms to shift. During this time, aim to swap out gluten-containing foods with naturally gluten-free whole foods rather than heavily processed alternatives. For example, instead of replacing wheat bread with gluten-free bread (which can be just as processed), opt for foods like sweet potatoes—they offer similar starch and fiber content, with more nutrients and fewer additives.
Keep in mind, one of the main ways gluten impacts gut health is by increasing intestinal permeability (leaky gut). Supporting your gut lining during this elimination phase by increasing anti-inflammatory, gut-healing foods can make a big difference. We highlight our top food recommendations in this article.

Making the Switch to Gluten-Free Made Easy with Metabolic Meals
Going gluten-free can be a powerful step toward improving your gut health and overall well-being. But navigating a gluten-free lifestyle can feel overwhelming, from reading labels to finding convenient, tasty options that fit your busy life.
That’s where Metabolic Meals comes in. We provide ready-made, delicious gluten-free meals designed to make your transition to a gluten-free lifestyle, effortless and enjoyable.
If you’re ready to take control of your gut health and experience the benefits of a gluten-free lifestyle without sacrificing convenience or flavor, Metabolic Meals is here to help every step of the way.
About the Author
Lauren Papanos is a licensed registered dietitian nutritionist and nutrition researcher, published in the Journal of Women’s Sports Medicine. She holds her bachelor’s and master’s degrees in nutrition sciences, board certification in sports nutrition as well as advanced certifications in functional medicine and functional endocrinology. She is the owner of the private practice, Functional Fueling Nutrition where they specialize in working with active women and athletes with thyroid diseases and endocrine and metabolic conditions. Lauren has been featured on national television and in Forbes, Shape and Insider. She is the host of the Strength in Hormones Podcast. You can find Lauren on Instagram at functional.fueling and learn more about her practice at www.functionalfueling.com.






